With the prevalence of COVID-19 still in our communities, we would like to remind fellow Bruins of mitigation practices to reduce likelihood of infection. Topics covered below include reducing the risk of COVID-19, awareness of riskier situations, effectiveness of voluntary mask-wearing and information on long COVID. We want to thank and acknowledge the Undergraduate Student Association Council (USAC) and Disabled Student Union (DSU) for the advocacy in the development of this campaign in partnership with UCLA Administration and The Arthur Ashe Student Health & Wellness Center.
Should you have any questions, please feel free to contact covid19@ucla.edu.
Masking for COVID-19 Mitigation & Risk Reduction
Wearing Masks & Respirators
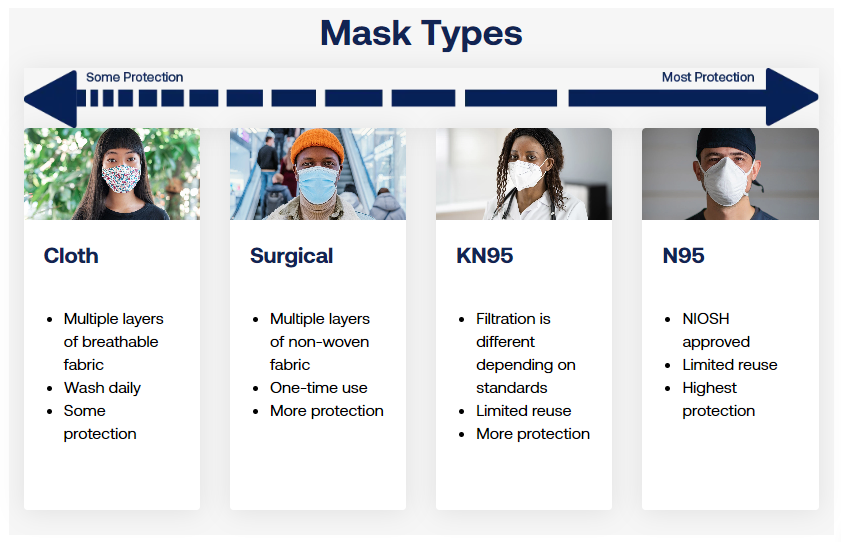
Masks are made to contain droplets and particles that you breathe, cough, or sneeze out. A variety of masks are available. Some masks provide a higher level of protection than others.
Respirators (for example, N95) are made to protect you by fitting closely on the face to filter out particles, including the virus that causes COVID-19. They can also block droplets and particles you breathe, cough, or sneeze out so you do not spread them to others. Respirators (for example, N95) provide higher protection than masks.
When wearing a mask or respirator (for example, N95), it is most important to choose one that you can wear correctly, that fits closely to your face over your mouth and nose, that provides good protection, and that is comfortable for you.
Reusing and Caring for Masks
Start each day with a clean mask.
Reusing Masks
- N95, KN95, or KF94 masks can be reused. Throw them away when they become wet, soiled, or damaged, if the straps become loose, or the mask no longer fits snugly.
- Medical/surgical paper masks can be used for one day. Throw them away at the end of each day, or sooner if they become wet, soiled, or damaged.
- Cloth masks can be reused if they are not damaged, and if they fit well and are washed daily.
Masking Indoors at UCLA
Wearing a well-fitting, highly protective face mask is still an effective and recommended precautionary measure against COVID-19, especially when indoors and in crowded areas.
As of May 1, 2024: Universal masking is no longer mandated, but it is suggested in healthcare settings.
Where to get masks on UCLA campus


Masks Help Protect People at Higher Risk
Wearing masks helps to protect everyone. When adults and children wear masks, they protect others who are at higher risk for severe illness. This includes babies under 6 months who are too young to be vaccinated against COVID-19 and children under 2 who cannot wear masks. This also includes children and staff who have immune problems, are affected by certain chronic illnesses or disabilities, or are not up to date on COVID-19 vaccinations. Early childhood programs may consider requiring masks at any time to protect people who are at higher risk of illness in their programs.
Some People Cannot Wear Masks
Masks should not be worn by:
- Children who are under 2 years old.
- Anyone who cannot remove their own mask.
- A child who has a special health care need and whose health care provider advises the family that their child should not wear a mask.
- People who cannot safely wear a mask because of a disability as defined by the Americans with Disabilities Act (ADA).
- People while they are eating or drinking, brushing teeth, resting, or sleeping.
Increasing Space and Distance
Small particles that people breathe out can contain virus particles. The closer you are to a greater number of people, the more likely you are to be exposed to the virus that causes COVID-19. To avoid this possible exposure, you may want to avoid crowded areas, or keep distance between yourself and others. These actions also protect people who are at high risk for getting very sick from COVID-19 in settings where there are multiple risks for exposure.
People Who Are Immunocompromised Are At Higher-Risk for Severe COVID-19
People who are moderately and severely immunocompromised are more likely to become severely ill with COVID-19. They may not be protected even if they are up to date on their COVID-19 vaccines and may need to take additional precautions to stay safe.
What does it mean to be immunocompromised? The immune system defenses are lowered and may not be able to fight off infections and diseases. This can be due to a medical condition or treatment for a medical condition.
What is Long COVID?
About Long COVID
Long COVID is a wide range of new, returning, or ongoing health problems that people experience after being infected with the virus that causes COVID-19. Most people with COVID-19 get better within a few days to a few weeks after infection, so at least 4 weeks after infection is the start of when Long COVID could first be identified. Anyone who was infected can experience Long COVID. Most people with Long COVID experienced symptoms days after first learning they had COVID-19, but some people who later experienced Long COVID did not know when they got infected.
There is no test that determines if your symptoms or condition is due to COVID-19. Long COVID is not one illness. Your healthcare provider considers a diagnosis of Long COVID based on your health history, including if you had a diagnosis of COVID-19 either by a positive test or by symptoms or exposure, as well as based on a health examination.